

It is safest to assume that where an allergic reaction has occurred, it is most likely to occur again on subsequent exposure, and the severity of the reaction may be similar or worse. Prior tolerance of a drug is not evidence against allergy to the drug, indeed, prior exposure is necessary for sensitisation. The principles of the natural history of drug allergy reactions are shown in Table 4. There may be an element of idiosyncrasy because there may be an underlying genetic polymorphism in those who are susceptible to this side-effect. Inhibition of angiotensin converting enzyme can lead to an excess of tissue bradykinin triggering angioedema, which is often thought of as an allergic disorder but in this case is related to the pharmacological effect of the drug. Pseudo-allergy refers to adverse reactions that produce clinical features that mimic allergy but are not mediated by immunological mechanisms. In these cases, genetic testing prior to drug administration will reduce the risk of ADRs. Genetic susceptibility may predispose to side-effects, intolerance reactions or allergic reactions ( Table 7). Idiosyncrasy is a term used to refer to an individual’s susceptibility to a drug ADR based on genetic variation. Extended Gell and Coombs classification TypeĭRESS (drug rash eosinophilia systemic symptoms)Īcute generalised exanthematous pustulosis
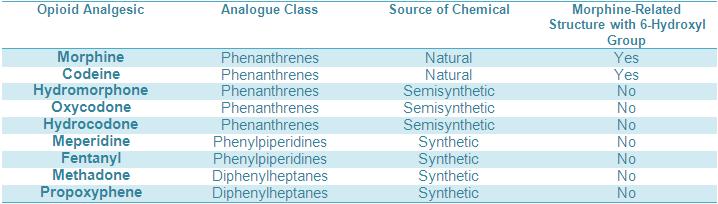
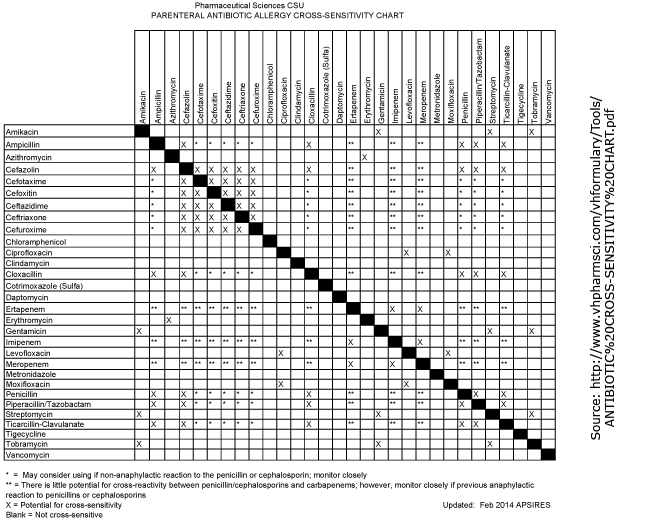
Opioid cross reactivity plus#
Pharmacological plus susceptibility unknown Terminology of adverse drug reaction mechanisms Classification The nature of the ADR may allow classification according to mechanism ( Table 2, Table 3). This will enable an assessment of the risk of future use of the drug and related medicines. Record in the patient file as much detail as possible regarding the ADR, rather than simply ‘allergy to drug X’ ( Table 1). The reaction may have been caused by an interaction between cofactors and the drug in question infection)Ĭould this have caused the reaction rather than the medication?Ĭofactors (eg.
May determine level of future contraindication Reaction severity, management required (eg. May allow classification of adverse drug reaction type Timing of onset and offset of reaction in relation to commencement and cessation of drug Side-effects, intolerance reactions may be dose-related Trade name relevant – excipients may rarely be involved in the reaction Generic and trade name of drug associated with adverse drug reaction Details of adverse drug reactions to be noted in the clinical record Detail
Opioid cross reactivity verification#
When a past reaction is described, verification and details should be sought from previous medical reports or contemporaneous records from other sources. In these cases, the medication thought to be causing the allergy will need to be stopped. However, it is usually not possible to test for drug allergy during the reaction, and the drug under suspicion (usually the most recently started) will need to be stopped.
Opioid cross reactivity skin#
For example, serum tryptase in the case of suspected anaphylaxis, eosinophilia in a chronic reaction, and skin biopsy in the case of a rash. Where allergy is suspected, testing may be helpful. In the setting of a current reaction, it is important to make a thorough assessment of the nature and severity of the ADR, and where not obvious, refer to available information on the known side-effects of the medication in question.


 0 kommentar(er)
0 kommentar(er)
